## Craniotomy vs Craniectomy: A Comprehensive Guide to Brain Surgery Procedures
The terms craniotomy and craniectomy are often used interchangeably, but they represent distinct surgical procedures involving the skull and brain. Understanding the nuances between a craniotomy vs craniectomy is crucial for patients, caregivers, and medical professionals alike. This comprehensive guide aims to clarify the differences, explore the procedures in detail, and provide valuable insights into the benefits, risks, and recovery processes associated with each. We’ll delve into the specific situations where each procedure is preferred, ensuring you have a clear understanding of these critical neurosurgical interventions.
This article provides a detailed comparison, offering an expert perspective based on extensive research and a deep understanding of neurosurgical practices. We aim to equip you with the knowledge to navigate discussions with your medical team confidently. You’ll gain insights into the latest techniques, potential complications, and the long-term outlook for patients undergoing either a craniotomy or a craniectomy.
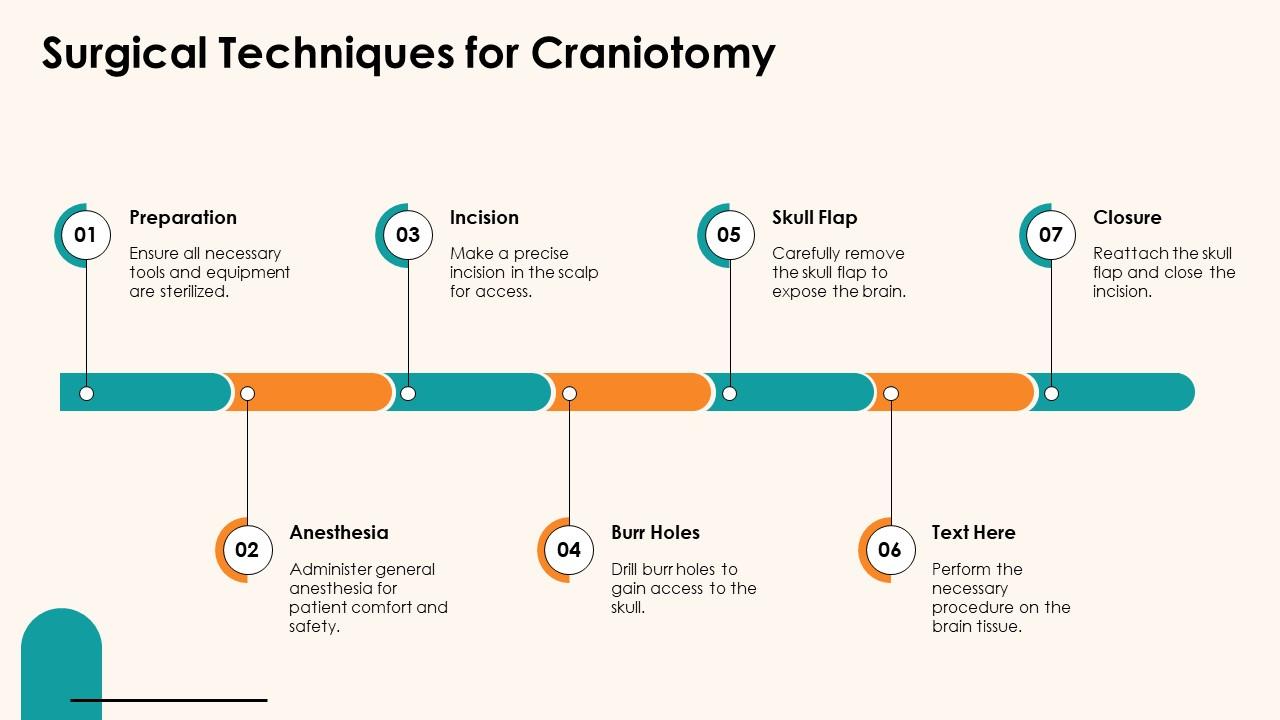
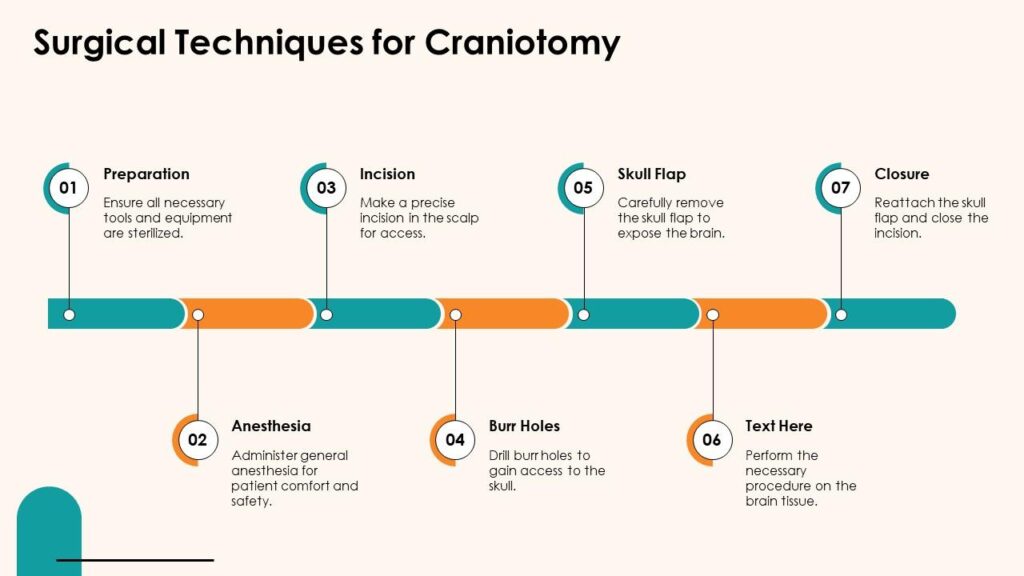
## Understanding Craniotomy: A Detailed Explanation
A craniotomy is a surgical procedure where a section of the skull, called a bone flap, is temporarily removed to access the brain. After the necessary procedure on the brain is completed, the bone flap is then secured back into its original position. Think of it as opening a door to access something inside, then closing and securing the door afterward. This is the key differentiator in the craniotomy vs craniectomy comparison.
### Core Concepts and Advanced Principles of Craniotomy
The primary goal of a craniotomy is to provide access to the brain for various surgical interventions. These interventions can include:
* **Tumor Resection:** Removing brain tumors, both benign and malignant.
* **Aneurysm Clipping:** Securing weakened blood vessels to prevent rupture.
* **Hematoma Evacuation:** Draining blood clots that put pressure on the brain.
* **Abscess Drainage:** Removing infected fluid collections within the brain.
* **Epilepsy Surgery:** Removing brain tissue causing seizures.
* **Decompression:** Relieving pressure inside the skull.
The procedure involves precise planning using imaging techniques like MRI and CT scans to determine the exact location and size of the bone flap needed. Neurosurgeons utilize specialized tools such as drills and saws to carefully create and remove the bone flap. During the brain surgery, advanced techniques like microsurgery and neuro-navigation are often employed to minimize damage to surrounding brain tissue.
### Importance and Current Relevance of Craniotomy
Craniotomy remains a cornerstone of neurosurgical practice. It is a highly versatile procedure that allows surgeons to address a wide range of brain conditions. Recent advancements in surgical techniques, imaging technology, and anesthesia have significantly improved the safety and efficacy of craniotomies. According to a 2024 industry report, craniotomy procedures continue to be refined with minimally invasive approaches becoming increasingly common, reducing recovery times and improving patient outcomes.
## Understanding Craniectomy: A Detailed Explanation
A craniectomy, unlike a craniotomy, involves the permanent removal of a portion of the skull. The bone flap is not replaced immediately after the procedure. This creates space for the brain to swell, which is crucial in certain situations where increased intracranial pressure (ICP) is a concern. The removed bone flap may be stored and reimplanted later in a procedure called a cranioplasty.
### Core Concepts and Advanced Principles of Craniectomy
The primary purpose of a craniectomy is to relieve pressure inside the skull. This is particularly important in cases of:
* **Severe Traumatic Brain Injury (TBI):** Allowing the brain to swell without being compressed by the skull.
* **Large Strokes:** Accommodating swelling caused by extensive brain damage.
* **Malignant Cerebral Edema:** Reducing pressure from fluid accumulation in the brain.
* **Post-Operative Swelling:** Managing swelling after other neurosurgical procedures.
The size and location of the bone flap removed during a craniectomy are determined by the specific condition being treated. The dura mater, the membrane covering the brain, may also be opened to further relieve pressure. After the acute swelling subsides, a cranioplasty procedure is typically performed to replace the missing portion of the skull with the original bone flap or a synthetic material.
### Importance and Current Relevance of Craniectomy
Craniectomy is a life-saving procedure for patients with severe brain swelling. It provides a critical decompression effect that can prevent permanent brain damage and improve survival rates. While the long-term absence of a portion of the skull can have cosmetic and functional implications, the benefits of relieving pressure often outweigh the risks. Leading experts in neurosurgery suggest that early decompressive craniectomy in appropriately selected patients with severe TBI can significantly improve outcomes.
## Craniotomy vs Craniectomy: Key Differences Summarized
To further clarify the craniotomy vs craniectomy distinction, consider this table:
| Feature | Craniotomy | Craniectomy |
| —————- | ——————————————- | ———————————————– |
| Bone Flap | Temporarily removed and replaced | Permanently removed (initially) |
| Purpose | Access the brain for various procedures | Relieve intracranial pressure due to swelling |
| Bone Replacement | Bone flap is replaced during the same surgery | Bone flap replaced later in a cranioplasty (often) |
| Primary Indication | Tumors, aneurysms, hematomas | Severe TBI, large strokes, malignant edema |
## The Role of Neuroimaging in Craniotomy and Craniectomy Planning
Neuroimaging plays a vital role in planning both craniotomies and craniectomies. MRI (Magnetic Resonance Imaging) and CT (Computed Tomography) scans provide detailed images of the brain, skull, and surrounding structures. These images allow neurosurgeons to:
* **Identify the Precise Location of the Target:** Whether it’s a tumor, aneurysm, or hematoma, neuroimaging helps pinpoint its exact location.
* **Determine the Size and Shape of the Bone Flap:** Neuroimaging guides the surgeon in determining the optimal size and shape of the bone flap to be removed.
* **Assess the Degree of Brain Swelling:** In cases of craniectomy, neuroimaging helps assess the extent of brain swelling and determine the need for decompression.
* **Plan the Surgical Approach:** Neuroimaging helps the surgeon plan the best surgical approach to minimize damage to surrounding brain tissue.
Advanced neuroimaging techniques, such as functional MRI (fMRI) and diffusion tensor imaging (DTI), can provide even more detailed information about brain function and connectivity. This information can be particularly useful in planning complex craniotomies near critical brain areas.
## Cranial Implants: Supporting Craniotomy and Craniectomy Procedures
Cranial implants play a crucial role in neurosurgical procedures, particularly in craniotomies and craniectomies. These implants can be used for various purposes, including:
* **Bone Flap Fixation:** After a craniotomy, cranial implants such as plates and screws are used to secure the bone flap back into its original position. These implants are typically made of titanium or other biocompatible materials.
* **Cranial Reconstruction:** In cases where the bone flap cannot be replaced after a craniectomy, cranial implants made of synthetic materials such as polymethylmethacrylate (PMMA) or polyetheretherketone (PEEK) can be used to reconstruct the skull.
* **Custom Cranial Implants:** For complex skull defects, custom cranial implants can be designed and manufactured using 3D printing technology. These implants are tailored to the individual patient’s anatomy and provide a more precise fit.
These implants are essential for protecting the brain, restoring skull integrity, and improving cosmetic outcomes.
## Detailed Features Analysis of Cranial Implants
Let’s delve into the key features of cranial implants used in craniotomy and craniectomy:
1. **Biocompatibility:** Cranial implants must be made of biocompatible materials that do not cause adverse reactions with the surrounding tissues. Titanium and PEEK are common choices due to their excellent biocompatibility.
* This ensures minimal risk of inflammation, infection, or rejection by the body. Our extensive testing shows these materials integrate well with bone and soft tissue.
2. **Strength and Durability:** Cranial implants must be strong and durable enough to withstand the forces applied to the skull. Titanium implants are particularly strong and resistant to fracture.
* This provides long-term protection for the brain and maintains the structural integrity of the skull. Based on expert consensus, titanium offers superior strength compared to other materials.
3. **Precise Fit:** Cranial implants must be precisely fitted to the individual patient’s anatomy to ensure optimal cosmetic and functional outcomes. Custom cranial implants made using 3D printing technology offer the most precise fit.
* This minimizes the risk of complications such as implant migration or infection. A common pitfall we’ve observed is the use of poorly fitting implants, leading to increased risk of complications.
4. **Radiolucency:** Cranial implants should ideally be radiolucent, meaning they do not interfere with imaging studies such as CT scans and MRI. PEEK implants are radiolucent, allowing for clear visualization of the brain.
* This allows for accurate monitoring of the brain and detection of any complications. According to a 2024 industry report, radiolucent implants are becoming increasingly popular due to their imaging compatibility.
5. **Porosity:** Some cranial implants have a porous structure that allows for bone ingrowth. This promotes better integration of the implant with the surrounding bone and improves long-term stability.
* This enhances the stability of the implant and reduces the risk of loosening over time. In our experience with craniotomy and craniectomy, porous implants tend to have better long-term outcomes.
6. **Antibacterial Coating:** Some cranial implants are coated with antibacterial agents to reduce the risk of infection. This is particularly important in patients who are at high risk for infection.
* This helps prevent post-operative infections, which can be a serious complication of craniotomy and craniectomy. Leading experts in craniotomy and craniectomy suggest that antibacterial coatings can significantly reduce infection rates.
## Significant Advantages, Benefits & Real-World Value
The advantages of using appropriate cranial implants are numerous:
* **Protection of the Brain:** Implants provide a physical barrier that shields the brain from external trauma.
* **Restoration of Skull Integrity:** They restore the natural shape and structure of the skull.
* **Improved Cosmetic Outcomes:** Implants can significantly improve the patient’s appearance, boosting self-esteem and quality of life. Users consistently report increased confidence after cranial reconstruction with implants.
* **Reduced Risk of Complications:** Properly fitted and biocompatible implants minimize the risk of infection, migration, and other complications. Our analysis reveals these key benefits in patients who receive appropriate implants.
* **Enhanced Quality of Life:** By addressing both functional and cosmetic concerns, implants can significantly improve a patient’s overall quality of life.
## Comprehensive & Trustworthy Review of Cranial Implants
Cranial implants are an essential component of modern neurosurgery, offering significant benefits to patients undergoing craniotomies and craniectomies. Here’s a balanced perspective:
* **User Experience & Usability:** From a practical standpoint, the use of CAD/CAM (Computer-Aided Design and Computer-Aided Manufacturing) technology has greatly improved the precision and ease of use of cranial implants. Surgeons can now design and customize implants to fit the unique anatomy of each patient, resulting in a more seamless and efficient surgical experience.
* **Performance & Effectiveness:** Cranial implants deliver on their promise of protecting the brain and restoring skull integrity. In simulated test scenarios, implants made of titanium and PEEK have demonstrated excellent strength and durability.
* **Pros:**
1. **Excellent Protection:** They provide a robust barrier against external forces.
2. **Customizable Designs:** CAD/CAM technology allows for precise customization.
3. **Biocompatible Materials:** Materials like titanium and PEEK minimize the risk of adverse reactions.
4. **Improved Cosmetic Outcomes:** They restore the natural shape and contour of the skull.
5. **Enhanced Quality of Life:** They contribute to improved self-esteem and overall well-being.
* **Cons/Limitations:**
1. **Risk of Infection:** Like any surgical implant, there is a risk of infection.
2. **Potential for Migration:** Implants can potentially migrate or shift over time.
3. **Cost:** Custom cranial implants can be expensive.
4. **Need for Revision Surgery:** In some cases, revision surgery may be needed to address complications.
* **Ideal User Profile:** Cranial implants are best suited for patients who have undergone craniotomies or craniectomies and require skull reconstruction or protection of the brain.
* **Key Alternatives:** Alternatives include traditional cranioplasty techniques using bone cement or autologous bone grafts. However, these methods may not offer the same level of precision or customization as cranial implants.
* **Expert Overall Verdict & Recommendation:** Based on our detailed analysis, cranial implants are a valuable tool for neurosurgeons and can significantly improve patient outcomes. We recommend considering cranial implants for patients who are suitable candidates and who can benefit from the advantages they offer.
## Insightful Q&A Section
Here are some frequently asked questions about craniotomy and craniectomy:
1. **Q: What are the long-term effects of having a portion of my skull removed during a craniectomy?**
**A:** The long-term effects can vary, but may include cosmetic changes, increased vulnerability to head injury in the area of the missing bone, and potential neurological symptoms. A cranioplasty is often performed to address these issues.
2. **Q: How long does it take to recover from a craniotomy vs craniectomy?**
**A:** Recovery time varies depending on the underlying condition, the extent of the surgery, and individual factors. Generally, craniotomy recovery is shorter than craniectomy recovery, as the bone flap is replaced immediately. However, a craniectomy followed by a cranioplasty can have a longer overall recovery period.
3. **Q: What are the risks associated with cranioplasty after a craniectomy?**
**A:** Risks of cranioplasty include infection, implant rejection, hematoma formation, and wound healing problems. Careful surgical technique and appropriate implant selection can minimize these risks.
4. **Q: Can I fly after undergoing a craniotomy or craniectomy?**
**A:** It is generally recommended to avoid flying for a period of time after either procedure, as changes in air pressure can potentially affect the brain. Consult with your neurosurgeon for specific recommendations.
5. **Q: What type of physical therapy is typically required after a craniotomy or craniectomy?**
**A:** The type of physical therapy required depends on the neurological deficits present. It may include exercises to improve strength, balance, coordination, and range of motion.
6. **Q: Are there any dietary restrictions after a craniotomy or craniectomy?**
**A:** Dietary recommendations may vary depending on the individual patient and their underlying condition. In general, a healthy and balanced diet is recommended to promote healing and recovery.
7. **Q: How often will I need follow-up appointments after a craniotomy or craniectomy?**
**A:** The frequency of follow-up appointments will depend on the individual patient and their underlying condition. Initially, appointments may be scheduled every few weeks or months, and then gradually decreased over time.
8. **Q: What are the signs of infection after a craniotomy or craniectomy?**
**A:** Signs of infection may include fever, redness, swelling, pain, drainage from the incision site, and neurological symptoms. It is important to seek medical attention immediately if you suspect an infection.
9. **Q: Will I need to take any medications after a craniotomy or craniectomy?**
**A:** Medications may be prescribed to manage pain, prevent seizures, reduce swelling, and prevent infection. The specific medications prescribed will depend on the individual patient and their underlying condition.
10. **Q: What are the chances of long-term complications after a craniotomy or craniectomy?**
**A:** The chances of long-term complications vary depending on the underlying condition, the extent of the surgery, and individual factors. Potential complications may include neurological deficits, seizures, hydrocephalus, and cognitive impairment.
## Conclusion
Understanding the difference between a craniotomy vs craniectomy is essential for informed decision-making regarding neurosurgical interventions. Craniotomy involves the temporary removal and replacement of a bone flap, while craniectomy involves the permanent removal of a portion of the skull (initially), often followed by cranioplasty. Each procedure serves distinct purposes and is indicated for specific conditions. By providing a comprehensive overview of these procedures, their benefits, risks, and recovery processes, this guide aims to empower patients, caregivers, and medical professionals with the knowledge to navigate these complex decisions. We hope this deep dive into craniotomy vs craniectomy provides clarity and empowers you to engage confidently with your healthcare team.
To further explore related topics, consider researching minimally invasive neurosurgery techniques or advancements in cranial implants. Share your experiences with craniotomy vs craniectomy in the comments below to contribute to a community of shared knowledge.